POSTERIOR HORN DETACHMENT OF THE MEDIAL MENSICUS
Posterior Detachment of the Medial Meniscus (PMD) is a meniscal tear not formerly described in the literature. This condition was first recognized at The Portland Knee Clinic in 1984 as a disruption of the extreme posterior attachment (ligamentous) of the medial meniscus (see Fig. 1). It tends to occur in patients after they enter the six decade (above 50 years) but has been observed in younger patients. It occurs occasionally in the lateral meniscus, but the preponderance of cases involve the medial meniscus. The posterior horn of the medial meniscus is the area of maximal stress during most activities and gradual weak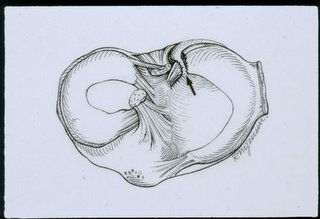 ening occurs at the posterior horn attachment in 7% of patients with medial meniscus injuries in stable knees. This is an attritional lesion. The knee is usually asymptomatic until the last fibers rupture, then, a seemingly minor event, such as stepping on to an escalator, arising from a chair or applying the car brakes can cause the final injury. When the posterior moorings finally go, the meniscus slides out of the joint with compressive load and the meniscus becomes almost totally non-functional (See Fig. 2).
ening occurs at the posterior horn attachment in 7% of patients with medial meniscus injuries in stable knees. This is an attritional lesion. The knee is usually asymptomatic until the last fibers rupture, then, a seemingly minor event, such as stepping on to an escalator, arising from a chair or applying the car brakes can cause the final injury. When the posterior moorings finally go, the meniscus slides out of the joint with compressive load and the meniscus becomes almost totally non-functional (See Fig. 2).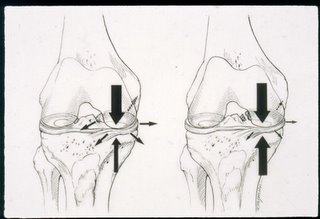 The medial compartment is instantly overloaded by forces usually absorbed by the hoop structure of the medial meniscus and severe medial pain develops. Frequently the patients come into the office on crutches. They are tender medially but frequently don't have an effusion or loss of motion. Plain standing x-rays are usually normal (Fig 3.) because this is an early lesion. The MRI is also usually normal because
The medial compartment is instantly overloaded by forces usually absorbed by the hoop structure of the medial meniscus and severe medial pain develops. Frequently the patients come into the office on crutches. They are tender medially but frequently don't have an effusion or loss of motion. Plain standing x-rays are usually normal (Fig 3.) because this is an early lesion. The MRI is also usually normal because this area is very hard to image. Sometimes on the axial views the lesion will be seen if the cut is just right. It can also be seen on the posterior coronal views occasionally by looking carefully at the medial meniscus right next to the PCL. If a bone scan is obtained, frequently one will see extreme uptake on the tibial side due to overloading. Prior to MRI it was impossible to distinguish this condition from the early stages of spontaneous osteonecrosis because of the uptake on the bone scan. However, SONC usually involves the femur, whereas the uptake with PMD usually occurs on the tibial side (Figure 4.)
this area is very hard to image. Sometimes on the axial views the lesion will be seen if the cut is just right. It can also be seen on the posterior coronal views occasionally by looking carefully at the medial meniscus right next to the PCL. If a bone scan is obtained, frequently one will see extreme uptake on the tibial side due to overloading. Prior to MRI it was impossible to distinguish this condition from the early stages of spontaneous osteonecrosis because of the uptake on the bone scan. However, SONC usually involves the femur, whereas the uptake with PMD usually occurs on the tibial side (Figure 4.)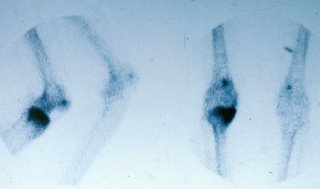 . The only way to be absolutely sure about the diagnosis is by arthroscopy.
. The only way to be absolutely sure about the diagnosis is by arthroscopy.
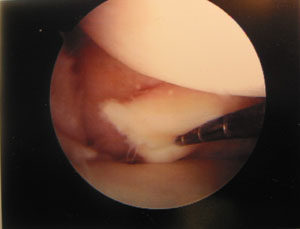
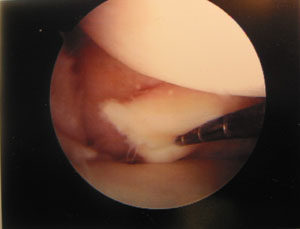
Because the posterior attachment of the medial meniscus curves around into the saddle of for the PCL and because it is so far back it is usually missed by the arthroscopist. This is the reason there has been no description of this lesion in the literature. Sometimes the extreme posterior horn has granulation tissue which has to be cleared. If the knee is tight it is more difficult to see posteriorly. The key is a good leg holder (Such as the Johnson) and careful probing. With careful probing the meniscus will be found to elevate too high off the tibia and it can be moved medially. When this is done, the disruption will be seen (Figure 5.).
 Several procedures have been developed to repair this lesion. One is with "T- fix" sutures, first passed through the posterior horn from the medial portal, then pulled through a bony tunnel much like the posterior anchor for a meniscal transplant (Fig 6.)
Several procedures have been developed to repair this lesion. One is with "T- fix" sutures, first passed through the posterior horn from the medial portal, then pulled through a bony tunnel much like the posterior anchor for a meniscal transplant (Fig 6.)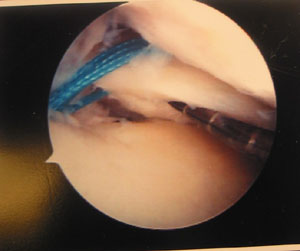 . Larger shoulder "T-fix" sutures provide solid fixation (Fig 7.). A blood clot has been used to aid healing. This procedure is not too difficult but has been only about 50% successful.
. Larger shoulder "T-fix" sutures provide solid fixation (Fig 7.). A blood clot has been used to aid healing. This procedure is not too difficult but has been only about 50% successful. 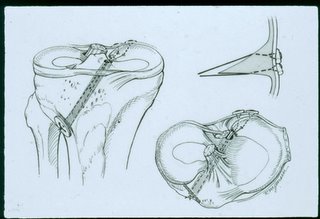 This is probably because the tissue quality is poor and there is extreme force in this area.
This is probably because the tissue quality is poor and there is extreme force in this area.
The second procedure is to attach the posterior horn to the PCL with "FastFix" sutures.
The third treatment is to roughen up the area, immobilize the knee and put the patient on crutches for 6 weeks.
Since this lesion is so common, the diagnosis is easy to make and in older patients, after full H&P, normal standing films, normal MRI and hot bone scan the patient can be put on crutches or a walker for six weeks and they frequently get better without surgery.
This lesion is the most common cause of a failed arthroscopy for medial pain or "tear of the medial meniscus".
About 50% of this patient group decompensate quickly and go on to a unicompartmental or total knee replacement.
A large number of total knee arthroplasties (TKA) are done at the Portland Knee Clinic and since becoming aware of this condition we have observed a high incidence of disruptions of the posterior horn in patients with medial osteoarthritis who are undergoing TKA. It takes a moment to assess the status of the meniscus before taking it out but the TKA surgeon will be surprised of how commonly it occurs. The body of the meniscus will look normal. There is usually an attempt by the natural repair process to heal this lesion and various levels of ineffective fibrous healing will be present. On close inspection it is noted that the posterior horn of the medial meniscus can easily be lifted off the tibia and displaced medially.
If an effective repair can be developed for PMD, possibly the incidence of medial osteoarthritis can be reduced.
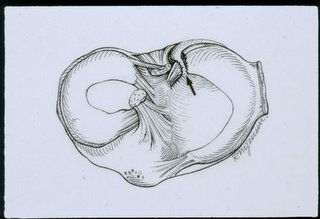 ening occurs at the posterior horn attachment in 7% of patients with medial meniscus injuries in stable knees. This is an attritional lesion. The knee is usually asymptomatic until the last fibers rupture, then, a seemingly minor event, such as stepping on to an escalator, arising from a chair or applying the car brakes can cause the final injury. When the posterior moorings finally go, the meniscus slides out of the joint with compressive load and the meniscus becomes almost totally non-functional (See Fig. 2).
ening occurs at the posterior horn attachment in 7% of patients with medial meniscus injuries in stable knees. This is an attritional lesion. The knee is usually asymptomatic until the last fibers rupture, then, a seemingly minor event, such as stepping on to an escalator, arising from a chair or applying the car brakes can cause the final injury. When the posterior moorings finally go, the meniscus slides out of the joint with compressive load and the meniscus becomes almost totally non-functional (See Fig. 2).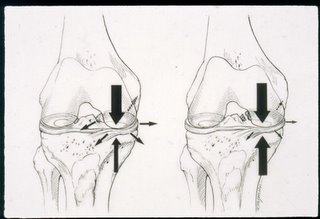 The medial compartment is instantly overloaded by forces usually absorbed by the hoop structure of the medial meniscus and severe medial pain develops. Frequently the patients come into the office on crutches. They are tender medially but frequently don't have an effusion or loss of motion. Plain standing x-rays are usually normal (Fig 3.) because this is an early lesion. The MRI is also usually normal because
The medial compartment is instantly overloaded by forces usually absorbed by the hoop structure of the medial meniscus and severe medial pain develops. Frequently the patients come into the office on crutches. They are tender medially but frequently don't have an effusion or loss of motion. Plain standing x-rays are usually normal (Fig 3.) because this is an early lesion. The MRI is also usually normal because this area is very hard to image. Sometimes on the axial views the lesion will be seen if the cut is just right. It can also be seen on the posterior coronal views occasionally by looking carefully at the medial meniscus right next to the PCL. If a bone scan is obtained, frequently one will see extreme uptake on the tibial side due to overloading. Prior to MRI it was impossible to distinguish this condition from the early stages of spontaneous osteonecrosis because of the uptake on the bone scan. However, SONC usually involves the femur, whereas the uptake with PMD usually occurs on the tibial side (Figure 4.)
this area is very hard to image. Sometimes on the axial views the lesion will be seen if the cut is just right. It can also be seen on the posterior coronal views occasionally by looking carefully at the medial meniscus right next to the PCL. If a bone scan is obtained, frequently one will see extreme uptake on the tibial side due to overloading. Prior to MRI it was impossible to distinguish this condition from the early stages of spontaneous osteonecrosis because of the uptake on the bone scan. However, SONC usually involves the femur, whereas the uptake with PMD usually occurs on the tibial side (Figure 4.)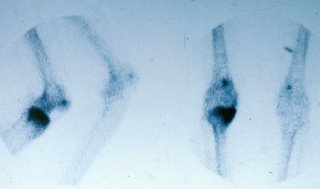 . The only way to be absolutely sure about the diagnosis is by arthroscopy.
. The only way to be absolutely sure about the diagnosis is by arthroscopy.Because the posterior attachment of the medial meniscus curves around into the saddle of for the PCL and because it is so far back it is usually missed by the arthroscopist. This is the reason there has been no description of this lesion in the literature. Sometimes the extreme posterior horn has granulation tissue which has to be cleared. If the knee is tight it is more difficult to see posteriorly. The key is a good leg holder (Such as the Johnson) and careful probing. With careful probing the meniscus will be found to elevate too high off the tibia and it can be moved medially. When this is done, the disruption will be seen (Figure 5.).
 Several procedures have been developed to repair this lesion. One is with "T- fix" sutures, first passed through the posterior horn from the medial portal, then pulled through a bony tunnel much like the posterior anchor for a meniscal transplant (Fig 6.)
Several procedures have been developed to repair this lesion. One is with "T- fix" sutures, first passed through the posterior horn from the medial portal, then pulled through a bony tunnel much like the posterior anchor for a meniscal transplant (Fig 6.)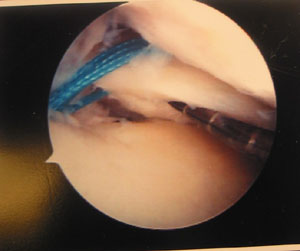 . Larger shoulder "T-fix" sutures provide solid fixation (Fig 7.). A blood clot has been used to aid healing. This procedure is not too difficult but has been only about 50% successful.
. Larger shoulder "T-fix" sutures provide solid fixation (Fig 7.). A blood clot has been used to aid healing. This procedure is not too difficult but has been only about 50% successful. 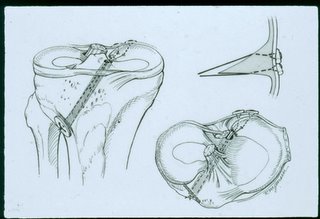 This is probably because the tissue quality is poor and there is extreme force in this area.
This is probably because the tissue quality is poor and there is extreme force in this area.The second procedure is to attach the posterior horn to the PCL with "FastFix" sutures.
The third treatment is to roughen up the area, immobilize the knee and put the patient on crutches for 6 weeks.
Since this lesion is so common, the diagnosis is easy to make and in older patients, after full H&P, normal standing films, normal MRI and hot bone scan the patient can be put on crutches or a walker for six weeks and they frequently get better without surgery.
This lesion is the most common cause of a failed arthroscopy for medial pain or "tear of the medial meniscus".
About 50% of this patient group decompensate quickly and go on to a unicompartmental or total knee replacement.
A large number of total knee arthroplasties (TKA) are done at the Portland Knee Clinic and since becoming aware of this condition we have observed a high incidence of disruptions of the posterior horn in patients with medial osteoarthritis who are undergoing TKA. It takes a moment to assess the status of the meniscus before taking it out but the TKA surgeon will be surprised of how commonly it occurs. The body of the meniscus will look normal. There is usually an attempt by the natural repair process to heal this lesion and various levels of ineffective fibrous healing will be present. On close inspection it is noted that the posterior horn of the medial meniscus can easily be lifted off the tibia and displaced medially.
If an effective repair can be developed for PMD, possibly the incidence of medial osteoarthritis can be reduced.


0 Comments:
Post a Comment
<< Home