Medial Subluxation of the Patella after Lateral Release
Lateral Retinacular Release has been in vogue for over fifty years as the treatment for patellofemoral problems associated with abnormal tightness of the structures that hold the patella ( knee cap) in place on the lateral side. The goal of this procedure is deminish the taughtness of these retaining structures whose function is to hold the patella in place and provide static control of tracking. Tightness of the lateral retinacular structures can lead to increased pressure in the lateral aspect of the patellofemoral joint and can cause a wide spectrum of problems from anterior knee pain to patellar dislocation. The former is a more benign form of the problem and the only symptom may be anterior pain (usually anterolaterally) with bent knee activities and the only finding a tight lateral retinacular ligament. More severe forms of the problem are associated with pain with a broad spectrum of activities and findings which may include patellar grinding (crepitation), decreased medial patellar excursion, lateral tracking of the patella and patellar tilting. In patients with associated genu valgus (knock knee), increased Q angle (angle between the vectors of the thigh muscle and the patellar tendon) and various degrees of extensor mechanism dysplasia (maldevelopment) the patella may actually dislocate. Lateral release alone is indicated in many of these circumstances except for those that involve dislocation. When dislocation is involved, lateral release plus more major realignment reconstruction (e.g. Trillat procedure) is indicated. If patients develop anterior knee pain and are diagnosed with tightness of the lateral retinaculum and do not improve with conservative treatment (exercises, medication, bracing, shoe devices) over a 12 to 18 month interval, then arthroscopic lateral release is indicated. At the time other minor procedures (such as smoothing the patella) can be done if needed.
When arthroscopic lateral release was first developed in the late 1970s and early 1980s some pioneers of the procedure recommended that it be done blindly with a pair of surgical scissors starting inferolaterally after enlarging the inferolateral arthroscopic portal. All of the lateral structures were severed until the patella could be stood on its side (everted), 90 degrees to its usual position. Some times this included cutting deeply into the vastus lateralis muscle. This technique turned out to be excessive in many cases and reports of medial subluxation (medial slippage) began to appear in the literature (e.g. Nonweiler & DeLee. AmJSportsMed 1994, 22[5]:680-686). With excessive lateral release, patients began to experience a spectrum of symptoms related to overpull of the medial structures: from medial patellofemoral pain to frank medial dislocation (See figure 1, right knee, medial dislocation). Over time procedures to reconstruct the lateral retinaculum to restore balance were developed ( e.g. Teitge. Arthroscopy 2004, 20[9]:998-1002). Procedures involving spaning a ligamentous structure from the lateral border of the patella to the lateral femoral condyle were found to be non-anatomic. Since the majority of the normal lateral retinacular ligament passes from the Iliotibial Band (ITB) to the lateral border of the bony patella, it seemed logical to recreate this anatomy rather than a bone to bone procedure. A procedure was developed at The Portland Knee Clinic to restore this normal anatomy by attaching a band of ligamentous tissue from the patella to the ITB, a surgery that allows the lateral forces to be modulated by the ITB, restoring stability but avoiding overtightening and recurrence of pain. The most suitable tissue for this reconstruction was found to be doubled fresh frozen iliotibial band. It is sewn to the retinaculum and periosteum of the anterior patella (2.5 cm wide) and to the ITB (4 cm wide) in a trapezoidal construct as shown in the attached photo (figure 2).
Over time procedures to reconstruct the lateral retinaculum to restore balance were developed ( e.g. Teitge. Arthroscopy 2004, 20[9]:998-1002). Procedures involving spaning a ligamentous structure from the lateral border of the patella to the lateral femoral condyle were found to be non-anatomic. Since the majority of the normal lateral retinacular ligament passes from the Iliotibial Band (ITB) to the lateral border of the bony patella, it seemed logical to recreate this anatomy rather than a bone to bone procedure. A procedure was developed at The Portland Knee Clinic to restore this normal anatomy by attaching a band of ligamentous tissue from the patella to the ITB, a surgery that allows the lateral forces to be modulated by the ITB, restoring stability but avoiding overtightening and recurrence of pain. The most suitable tissue for this reconstruction was found to be doubled fresh frozen iliotibial band. It is sewn to the retinaculum and periosteum of the anterior patella (2.5 cm wide) and to the ITB (4 cm wide) in a trapezoidal construct as shown in the attached photo (figure 2). 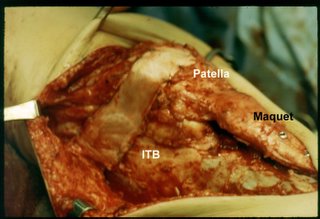 This has been quite sucessful in a number of cases and has been used to rebalance the extensor mechanism in other situations in which the lateral retinaculum has been found to be deficient. In the case shown here the synovium was plicated, the VLO repaired and a Maquet performed in addition to the LPFL reconstruction.
This has been quite sucessful in a number of cases and has been used to rebalance the extensor mechanism in other situations in which the lateral retinaculum has been found to be deficient. In the case shown here the synovium was plicated, the VLO repaired and a Maquet performed in addition to the LPFL reconstruction.
It is now understood that arthroscopic lateral release is carried out under direct vision with electrocautery from the inferior border of the vastus lateralis tendon proximally, through the lateral meniscopatellar ligament (Ficat & Hungerford. Disorders of the Patello-femoral Joint. p. 17. Williams and Wilkins 1977) distally. This seldom creates problems unless the lateral release is done in the presence of normal patellofemoral soft tissue balance.
When arthroscopic lateral release was first developed in the late 1970s and early 1980s some pioneers of the procedure recommended that it be done blindly with a pair of surgical scissors starting inferolaterally after enlarging the inferolateral arthroscopic portal. All of the lateral structures were severed until the patella could be stood on its side (everted), 90 degrees to its usual position. Some times this included cutting deeply into the vastus lateralis muscle. This technique turned out to be excessive in many cases and reports of medial subluxation (medial slippage) began to appear in the literature (e.g. Nonweiler & DeLee. AmJSportsMed 1994, 22[5]:680-686). With excessive lateral release, patients began to experience a spectrum of symptoms related to overpull of the medial structures: from medial patellofemoral pain to frank medial dislocation (See figure 1, right knee, medial dislocation).
 Over time procedures to reconstruct the lateral retinaculum to restore balance were developed ( e.g. Teitge. Arthroscopy 2004, 20[9]:998-1002). Procedures involving spaning a ligamentous structure from the lateral border of the patella to the lateral femoral condyle were found to be non-anatomic. Since the majority of the normal lateral retinacular ligament passes from the Iliotibial Band (ITB) to the lateral border of the bony patella, it seemed logical to recreate this anatomy rather than a bone to bone procedure. A procedure was developed at The Portland Knee Clinic to restore this normal anatomy by attaching a band of ligamentous tissue from the patella to the ITB, a surgery that allows the lateral forces to be modulated by the ITB, restoring stability but avoiding overtightening and recurrence of pain. The most suitable tissue for this reconstruction was found to be doubled fresh frozen iliotibial band. It is sewn to the retinaculum and periosteum of the anterior patella (2.5 cm wide) and to the ITB (4 cm wide) in a trapezoidal construct as shown in the attached photo (figure 2).
Over time procedures to reconstruct the lateral retinaculum to restore balance were developed ( e.g. Teitge. Arthroscopy 2004, 20[9]:998-1002). Procedures involving spaning a ligamentous structure from the lateral border of the patella to the lateral femoral condyle were found to be non-anatomic. Since the majority of the normal lateral retinacular ligament passes from the Iliotibial Band (ITB) to the lateral border of the bony patella, it seemed logical to recreate this anatomy rather than a bone to bone procedure. A procedure was developed at The Portland Knee Clinic to restore this normal anatomy by attaching a band of ligamentous tissue from the patella to the ITB, a surgery that allows the lateral forces to be modulated by the ITB, restoring stability but avoiding overtightening and recurrence of pain. The most suitable tissue for this reconstruction was found to be doubled fresh frozen iliotibial band. It is sewn to the retinaculum and periosteum of the anterior patella (2.5 cm wide) and to the ITB (4 cm wide) in a trapezoidal construct as shown in the attached photo (figure 2). 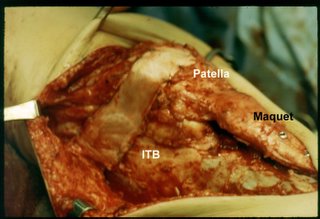 This has been quite sucessful in a number of cases and has been used to rebalance the extensor mechanism in other situations in which the lateral retinaculum has been found to be deficient. In the case shown here the synovium was plicated, the VLO repaired and a Maquet performed in addition to the LPFL reconstruction.
This has been quite sucessful in a number of cases and has been used to rebalance the extensor mechanism in other situations in which the lateral retinaculum has been found to be deficient. In the case shown here the synovium was plicated, the VLO repaired and a Maquet performed in addition to the LPFL reconstruction.It is now understood that arthroscopic lateral release is carried out under direct vision with electrocautery from the inferior border of the vastus lateralis tendon proximally, through the lateral meniscopatellar ligament (Ficat & Hungerford. Disorders of the Patello-femoral Joint. p. 17. Williams and Wilkins 1977) distally. This seldom creates problems unless the lateral release is done in the presence of normal patellofemoral soft tissue balance.


1 Comments:
Excellent post. Its really very effective and helpful. Thanks.
Emergency dental services Manhattan
NY
emergency dental clinic Manhattan NY
24 hour emergency dental office Manhattan
NY
Post a Comment
<< Home