The Anatomy and Kenematics
of the
Medial
Patellofemoral Ligament
James L. Baldwin, MD
It has been shown that the medial patellofemoral ligament (MPFL) is responsible for 60% of the medial restraining force of the patella [Desio SM. AJSM 1998;26:59-65] and that it is ruptured in virtually every acute patellar dislocation [Nomura E. The Knee 2002;9:139-143]. The treatment of patellar instability has been hampered by a lack of concensus about the true anatomy of the the MPFL. To clarify the anatomy of the MPFL, 69 human knee specimens were dissected between 2002 and 2004. None of the knees had significant pathology. After the first 19 dissections the study was restarted because of new findings. The last 50 knees comprise the basis for this study.
 The dissection is approached through an midline anterior longitudinal incision that is "L"ed proximally and distally. It was found that the skin and subcutaneous tissue are best separated from layer I by blunt dissection with an finger or sponge (Figure 1). In the laboratory this is accomplished nicely by attaching Leahy clamps (Gall Bladder Clamps) to the skin and subcutaneous tissue and applying firm traction to define the interval between the areolar tissue and the investing fascia. Attempting to expose layer I by sharp dissection or from the wrong location will usually violate layer I because it is adhered closely to the subcutaneous fat. When this happens, layer II, the home of the MPFL, can be injured.
The dissection is approached through an midline anterior longitudinal incision that is "L"ed proximally and distally. It was found that the skin and subcutaneous tissue are best separated from layer I by blunt dissection with an finger or sponge (Figure 1). In the laboratory this is accomplished nicely by attaching Leahy clamps (Gall Bladder Clamps) to the skin and subcutaneous tissue and applying firm traction to define the interval between the areolar tissue and the investing fascia. Attempting to expose layer I by sharp dissection or from the wrong location will usually violate layer I because it is adhered closely to the subcutaneous fat. When this happens, layer II, the home of the MPFL, can be injured.  It is best to tent and enter layer I posterior to the MCL and distal to the medial epicondyle. A blunt intrument is then used to separate and explore the interval between layer I and II (Figure 2). There are many and varied fibrous conections between layer I and II anterior to the medial collateral ligament (MCL).
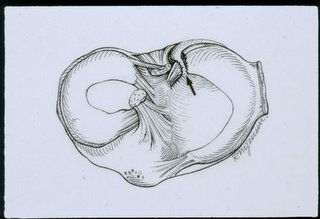
It is best to tent and enter layer I posterior to the MCL and distal to the medial epicondyle. A blunt intrument is then used to separate and explore the interval between layer I and II (Figure 2). There are many and varied fibrous conections between layer I and II anterior to the medial collateral ligament (MCL). Layer I is then tented and split longitudinally behind the MCL and reflected where possible. Note in figure 3 that there is a neurovascular complex separating layer I from layer II. These are the capsular branches of the descending genicular artery which is the last branch of the superficial femoral artery just before it passes through the adductor hiatus (Figure 4).
Layer I is then tented and split longitudinally behind the MCL and reflected where possible. Note in figure 3 that there is a neurovascular complex separating layer I from layer II. These are the capsular branches of the descending genicular artery which is the last branch of the superficial femoral artery just before it passes through the adductor hiatus (Figure 4).The first branch of the DGA is the saphenous artery which joins the saphenous nerve and travels behind the sartorius muscle. The DGA then passes down the intermuscular septum, giving off several muscular brances to the VMO and then its capsular branches that come to lie on top of the MPFL and is the key to the dissection. After the capsular branch, the DGA continues on to anastamose with the superior medial geniculate artery which then sends osseous brances to the femur. One of the main brances passes under the origin of the transverse portion of the MPFL, so the MPFL is literally "sandwiched" between two vessels. As long as the vessels are undisturbed the ligament will not be injured.
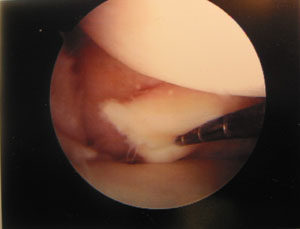
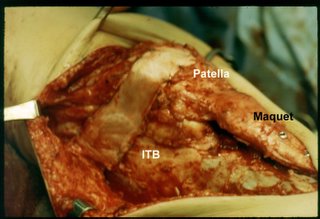
 Before proceding further the distal border of the vastus medial obliquus (VMO) is lifted to expose the sharp upper edge of the MPFL (Figure 5). The ligament then can be traced back its attachment on the femur with a blunt instrument. This allows the ligament to be tensioned, protected and defined.
Before proceding further the distal border of the vastus medial obliquus (VMO) is lifted to expose the sharp upper edge of the MPFL (Figure 5). The ligament then can be traced back its attachment on the femur with a blunt instrument. This allows the ligament to be tensioned, protected and defined.  Following the vessels (figure 6), it is found that the upper vessels lay on top of the transverse portion of the MPFL and the lower branches lay over the oblique portion of the MPFL that arises from the upper MCL. Note that a branch of the superior medial genicualte artery passes under the transverse portion of the MPFL separating it from the medial epicondyle, sandwiching the MPFL between the two vessels.
Following the vessels (figure 6), it is found that the upper vessels lay on top of the transverse portion of the MPFL and the lower branches lay over the oblique portion of the MPFL that arises from the upper MCL. Note that a branch of the superior medial genicualte artery passes under the transverse portion of the MPFL separating it from the medial epicondyle, sandwiching the MPFL between the two vessels.  The configuration seen in Figure 7 was seen in all patients except one. It is thought that the one case in which the decussation was not seen, it was damaged in elevating layer I off of layer II. The origin of the MPFL is dual. The upper transverse portion arises from the bony groove between the medial epicondyle and the adductor tubercle (Figure 8).
The configuration seen in Figure 7 was seen in all patients except one. It is thought that the one case in which the decussation was not seen, it was damaged in elevating layer I off of layer II. The origin of the MPFL is dual. The upper transverse portion arises from the bony groove between the medial epicondyle and the adductor tubercle (Figure 8).  It is 12 mm high, strong and ribbonlike. The oblique origin arises from the upper 3 cm of the MCL, is also ribbonlike and equal in strength to the transverse portion of the ligament. The two origins combine anterior to the medial epicondyle and form a broad ligament that is 4 cm wide.
It is 12 mm high, strong and ribbonlike. The oblique origin arises from the upper 3 cm of the MCL, is also ribbonlike and equal in strength to the transverse portion of the ligament. The two origins combine anterior to the medial epicondyle and form a broad ligament that is 4 cm wide.  As the MCL approaches the patella it combines inseparably with the tendon of the VMO and together they insert strongly into the most ventral aspect of the medial border of the patella all along its articular surface (Figure 9.).
As the MCL approaches the patella it combines inseparably with the tendon of the VMO and together they insert strongly into the most ventral aspect of the medial border of the patella all along its articular surface (Figure 9.).  The length of the MPFL from the groove to the medial border of the patella is 60 mm (Figure 10). Typical anatomy is again seen in this photograph. Layer I has been reflected where possible and layer II is seen and includes the MCL, the MPFL and the medial patellotibial ligament. There is no structure that can be called the medial retinaculum. The medial retinaculum is a general term that should be used to refer to the ligamentous structures on the medial side that stabilize the patella [Starok, M. AJR 1997;168:1493-1499].
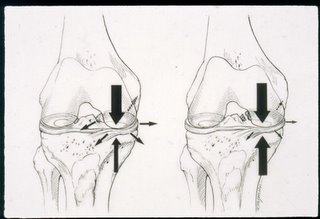
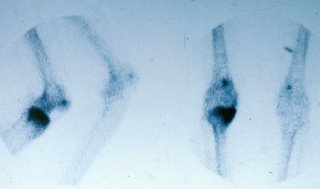
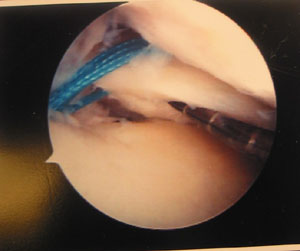
The length of the MPFL from the groove to the medial border of the patella is 60 mm (Figure 10). Typical anatomy is again seen in this photograph. Layer I has been reflected where possible and layer II is seen and includes the MCL, the MPFL and the medial patellotibial ligament. There is no structure that can be called the medial retinaculum. The medial retinaculum is a general term that should be used to refer to the ligamentous structures on the medial side that stabilize the patella [Starok, M. AJR 1997;168:1493-1499]. When the patella dislocates, the MPFL ruptures at is femoral orgin, its weakest link (Figure 11). The oblique portion of the ligament with its soft origin from the MCL dampens the lateral displacement of the patella and guides the transverse portion of the MPFL back to its origin. The MPFL seldom rupures from its strong attachment to the medial patella. When ossicles are seen on the medial side of the patella after a dislocation has occurred, they are usually avulsion fractures of the inferior medial pole of the patella where the medial patellotibial ligament (in layer III) attaches as opposed to avulsions of the conjoined tendon of the VMO and the MPFL off of the medial border of the patella.
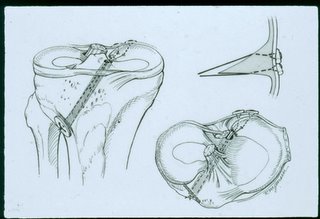
When the patella dislocates, the MPFL ruptures at is femoral orgin, its weakest link (Figure 11). The oblique portion of the ligament with its soft origin from the MCL dampens the lateral displacement of the patella and guides the transverse portion of the MPFL back to its origin. The MPFL seldom rupures from its strong attachment to the medial patella. When ossicles are seen on the medial side of the patella after a dislocation has occurred, they are usually avulsion fractures of the inferior medial pole of the patella where the medial patellotibial ligament (in layer III) attaches as opposed to avulsions of the conjoined tendon of the VMO and the MPFL off of the medial border of the patella.  In summary (Figure 12), the MPFL was present in all specimens. It has a dual origin. The transverse portion arising from the grove between the adductor tubercle and the medial epicondyle and an oblique portion arising from the upper edge of the MCL. Together they form a broad ligament which combines inseparably with the tendon of the VMO and together they insert strongly into the medial border of the patella all along it articular surface. The MPFL is entirely in Layer II and is defined by vessels that lay on its surface and under its origin. This percise anatomical information will aid the orthopedic surgeon in diagnosis and treatment of patellar instability.
In summary (Figure 12), the MPFL was present in all specimens. It has a dual origin. The transverse portion arising from the grove between the adductor tubercle and the medial epicondyle and an oblique portion arising from the upper edge of the MCL. Together they form a broad ligament which combines inseparably with the tendon of the VMO and together they insert strongly into the medial border of the patella all along it articular surface. The MPFL is entirely in Layer II and is defined by vessels that lay on its surface and under its origin. This percise anatomical information will aid the orthopedic surgeon in diagnosis and treatment of patellar instability.